In a recently published case report, a 54-year-old man from Florida has been diagnosed with leprosy, contributing to the increasing number of cases identified in the southeastern United States. This region is emerging as a new focal point for the disease.
This comes after recent alerts issued by the US Centers for Disease Control and Prevention (CDC) regarding the first instances of locally acquired malaria in the US in two decades, with four cases reported in Florida.
The incidence of leprosy, indicating the rates of new cases, has been on the rise in the southern regions of the US since 2000. Over the past decade, reported cases have more than doubled in the southeastern states, with Central Florida now representing nearly one-fifth of all cases in the United States.
However, a decreasing percentage of leprosy cases in the US are identified in individuals born outside the country. Simultaneously, there is a notable increase in reported cases that seem to lack the typical risk factors associated with the disease.
“Those trends,” wrote the three dermatologists who alerted public health officials to the Florida man’s diagnosis, “contribute to rising evidence that leprosy has become endemic in the south-eastern United States.”
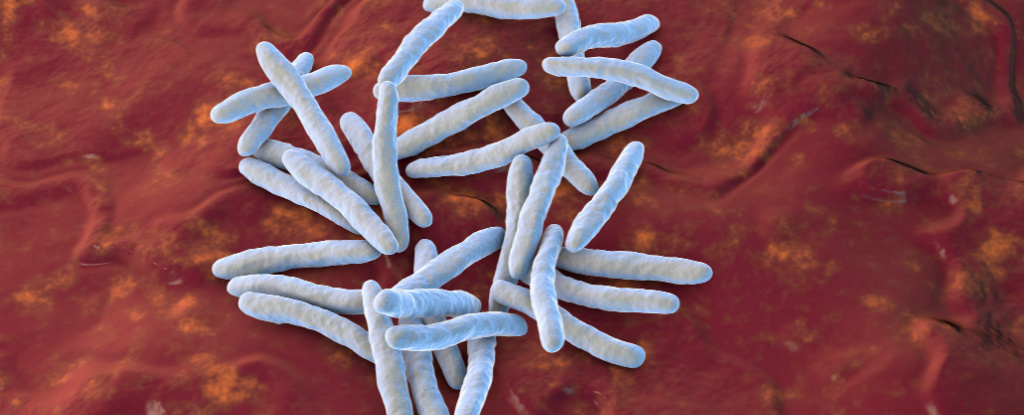
Leprosy, also recognized as Hansen’s disease, results from a bacterial infection caused by Mycobacterium leprae and the more recently identified M. lepromatosis. While it is a curable yet neglected tropical disease, entirely treatable with proper care, it remains prevalent in over 120 countries.
Approximately 150 cases of leprosy are reported in the US annually. While unique strains of M. leprae have been identified in US patients, the majority of cases involve individuals who have traveled from countries where leprosy is present or endemic.
According to the researchers, additional risk factors include exposure to animals such as nine-banded armadillos, which are known to harbor M. leprae, and prolonged, close contact over months with someone who has untreated leprosy. The disease is spread via droplets from the nose and mouth.
However, the 54-year-old man, a lifelong Florida resident, informed contact tracers that he had not traveled recently, nor had contact with someone known to have leprosy or any armadillos. Despite this, he works as a landscaper and spends a significant amount of time outdoors.
The man visited a dermatology clinic with a painful rash and skin lesions that initially surfaced on his feet and arms, later advancing to his trunk and face.
Biopsies substantiated the leprosy diagnosis, prompting the notification of public health officials by national protocols.
The man’s case, akin to around one-third of new leprosy cases identified in the US from 2015 to 2020, seems to have originated locally.
“Our case adds to the growing body of literature suggesting that central Florida represents an endemic location for leprosy,” dermatologists Aashni Bhukhan, Charles Dunn, and Rajiv Nathoo stated in their case report, published in August.
“By increasing local physician efforts to report the incidence and supporting further research to assess routes of transmission, a congruent effort can be made to identify and reduce the spread of the disease.”
Specifically, the lack of identified risk factors in recent leprosy cases in Florida, involving individuals spending time outdoors, has led researchers to explore potential environmental sources of the bacterial disease.
“The transmission of this disease is probably much more complicated than was thought before,” note the authors of a recent systematic review, which examined global leprosy transmission data published from 1945 to 2019.
It suggests a growing contribution of anthroponotic (human-to-human) and zoonotic (animal-to-human) transmission in the spread of leprosy.
The second confirmed cause of leprosy, M. lepromatosis, was identified only in 2008, 150 years after the disease was initially attributed to M. leprae.
Scientists are working to determine the prevalence of M. lepromatosis infections and identify the animals from which it may transfer to humans.
“It is perhaps remarkable that a new [bacterial] species causing an endemic disease of major public health impact has not prompted larger-scale studies to determine its true prevalence,” researchers remark.
The report on the Florida case has been released in Emerging Infectious Diseases.