Examination of human brain tissue uncovers distinctions in the behavior of immune cells within brains afflicted by Alzheimer’s disease when compared to healthy brains, suggesting a potential new target for treatment.
Research led by the University of Washington and published in August revealed that microglia in the brains of individuals with Alzheimer’s disease were more frequently in a pre-inflammatory state, diminishing their likelihood of being protective.
Microglia are immune cells crucial for maintaining the health of our brains, as they play a key role in clearing waste and preserving normal brain function.
In response to infection or the need to eliminate dead cells, these versatile shape-shifters can transition to a more mobile form, enabling them to engulf invaders and debris. Additionally, they engage in ‘pruning’ synapses during development, a process that contributes to shaping the neural circuitry necessary for optimal brain function.
While their role in Alzheimer’s is not fully understood, in individuals affected by this severe neurodegenerative disease, certain microglia exhibit an excessive response, potentially leading to inflammation that contributes to the death of brain cells.
Regrettably, trials of anti-inflammatory medications for Alzheimer’s have not demonstrated significant effects.
To explore the involvement of microglia in Alzheimer’s disease, neuroscientists Katherine Prater and Kevin Green from the University of Washington, along with collaborators from various US institutions, employed brain autopsy samples from research donors. The study included 12 individuals with Alzheimer’s and 10 healthy controls, aiming to analyze the gene activity of microglia.
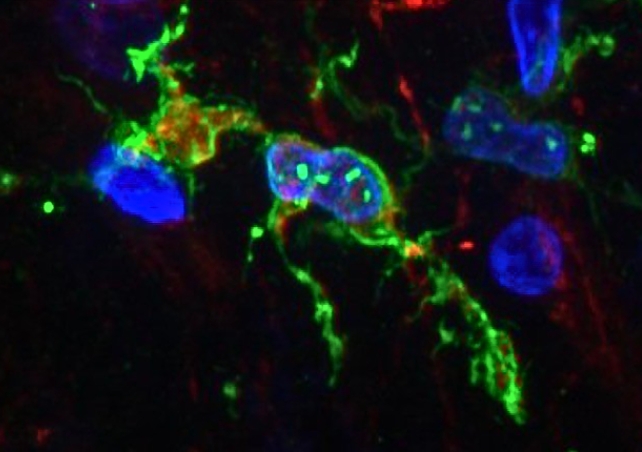
Employing an innovative approach to enhance single-nucleus RNA sequencing, the team successfully conducted an in-depth analysis, identifying 10 distinct clusters of microglia in the brain tissue based on their unique gene expression patterns, guiding the cells’ functions.
Among the identified clusters, three were previously undiscovered, and one of them exhibited a higher prevalence in individuals with Alzheimer’s disease. This particular microglia type displays activated genes associated with inflammation and cell death.
In summary, the researchers observed that microglia clusters in the brains of individuals with Alzheimer’s disease were more inclined to be in a pro-inflammatory state.
This implies that they were more prone to generate inflammatory molecules capable of harming brain cells and potentially playing a role in the advancement of Alzheimer’s disease.
The identified microglia types in the brains of individuals with Alzheimer’s disease exhibited a reduced likelihood of being protective, hampering their effectiveness in clearing dead cells and waste and fostering healthy brain aging.
The researchers also posit that microglia can change type over time. Therefore, merely examining a person’s brain may not definitively determine the type of microglia they have. Monitoring the evolution of microglia over time could provide insights into their role in contributing to Alzheimer’s disease.
“At this point, we can’t say whether the microglia are causing the pathology or whether the pathology is causing these microglia to alter their behavior,” said Prater.
While still in its preliminary phases, this research contributes to our comprehension of the role of these cells in Alzheimer’s disease and indicates that specific microglia clusters could be potential targets for novel treatments.
The team is optimistic that their efforts will pave the way for the creation of new therapies aimed at enhancing the lives of individuals with Alzheimer’s disease.
“Now that we have determined the genetic profiles of these microglia, we can try to find out exactly what they are doing and hopefully identify ways to change their behaviors that may be contributing to Alzheimer’s disease,” Prater said.
“If we can determine what they are doing, we might be able to change their behavior with treatments that might prevent or slow this disease.”
The research findings have been published in Nature Aging.