An estimated approximately 3% of individuals in the UK undergo the challenges of long COVID – enduring persistent symptoms following a COVID-19 infection.
Long COVID encompasses a variety of health issues that may emerge following even a mild COVID-19 infection. Among these symptoms are profound fatigue, breathlessness, muscle aches, and anosmia (loss of smell).
Approximately 50% of individuals with long COVID experience symptoms that align with the criteria for a diagnosis of myalgic encephalomyelitis (ME), a neuro-immune disease characterized by diminished energy, muscle weakness and pain, cognitive dysfunction, and dysautonomia, affecting blood pressure and heart rate.
An essential characteristic of ME is “post-exertional malaise” (PEM). This refers to a deterioration of symptoms occurring approximately 24-48 hours after any form of exertion—whether physical, cognitive, or emotional. PEM may persist for days or weeks.
PEM remains one of the most debilitating yet least understood features of both ME and long COVID. However, recent research may provide a likely explanation for why physical activity, in particular, exacerbates long COVID symptoms. The study revealed that individuals with long-term COVID show changes in their muscle structure.
To conduct their study, the researchers examined muscle biopsies and blood plasma samples collected from 25 individuals with long COVID and 21 people who had experienced COVID but did not develop long COVID. On average, participants in both groups were around 41 years old, with a nearly equal split between men and women (48% to 52%).
The blood and muscle samples were collected before and after a controlled cycling test. Participants engaged in cycling for about 15 minutes, beginning at a slow pace and gradually intensifying.
During the cycling test, individuals with long COVID demonstrated weaker muscular strength and lower oxygen uptake compared to the healthy participants, despite expending the same amount of effort. These findings align with previous studies, indicating a significant reduction in exercise capacity among people with long COVID.
Upon analyzing the participants’ muscle samples, the researchers observed that individuals with long COVID-19 had an increased proportion of fast-twitch glycolytic muscle fibers.
These muscle fibers can operate at high intensity in short bursts but are highly fatigable due to having fewer mitochondria, the organelles that supply cells with the energy they require to function properly.
The researchers subsequently conducted additional tests on the mitochondria in these fibers. They discovered that exercise diminished mitochondrial function in individuals with long-term COVID-19, suggesting that, in addition to having a reduced exercise capacity, their muscle tissue sustained damage during the exercise test.
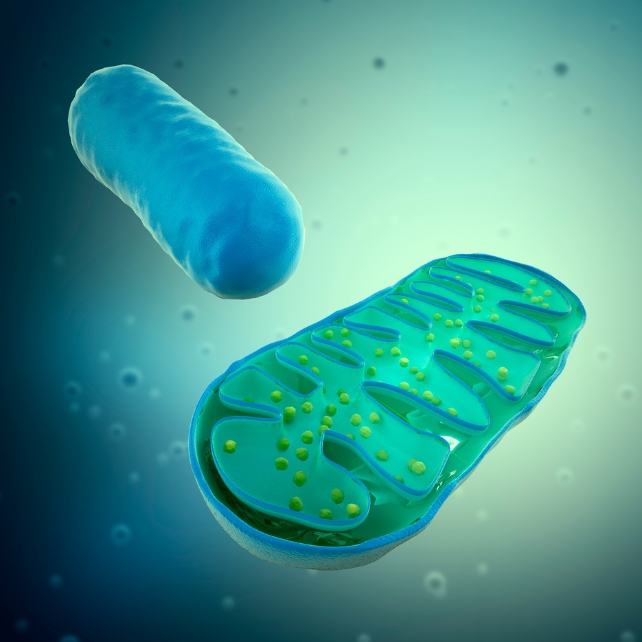
Examinations of molecules in muscle and plasma also indicated that individuals with long COVID exhibited reduced levels of essential molecules necessary for glycolysis, the process by which mitochondria supply cells with energy.
This is not the initial instance where mitochondrial dysfunction has been associated with an ailment featuring PEM. This theory was first proposed as the underlying mechanism in ME over 40 years ago.
If the mitochondria in muscles are not functioning properly, it indicates that muscle cells fail to generate sufficient energy to meet the body’s demands. This could elucidate why individuals with long COVID encounter exacerbated symptoms post-exercise.
Muscle ‘micro clots’
Subsequently, the researchers examined the muscle samples to determine the presence of clusters of misfolded proteins.
Prior research indicates the presence of clusters, known as “microclots,” which are elevated in the plasma of individuals with long COVID. It has been suggested that these microclots may obstruct capillaries, leading to tissue damage as blood reenters, potentially harming the mitochondria.
The researchers demonstrated that individuals with long COVID exhibited a higher presence of microclots in their muscles compared to the control group. The number of micro clots also rose after exercise in all participants, although there was no evidence indicating that they were obstructing capillaries.
Lastly, they examined the immune cells present in muscle tissue. They observed increased numbers of macrophages and T-cells, both of which contribute to tissue repair, in the samples of individuals with long COVID – even before engaging in exercise.
This suggests that individuals with long-term COVID exhibit activated immune cells in their muscle tissue, responding to the damage within the tissue.
It is recognized that inflammation, which can result from an overactive immune system, can both instigate and be a consequence of mitochondrial damage. This could be an additional factor contributing to the dysfunction of mitochondria in individuals with long-term COVID.
Targeting mitochondria
This study contributes to an expanding body of research highlighting significant irregularities in the metabolic, muscular, and immune functions among individuals with long COVID (and, by extension, those with ME). It also indicates that addressing the mitochondria may hold promise for alleviating symptoms.
Encouragingly, numerous compounds have demonstrated a positive impact on mitochondrial function. Certain options, like coenzyme Q10 (naturally produced in our bodies), are accessible without a prescription.
However, to determine if these compounds indeed impact long-term COVID symptoms, controlled trials with placebos must be conducted.
These results underscore the need for caution in crafting rehabilitation approaches for individuals with long-term COVID.
Conventional programs assume that gradual intensification improves resilience and exercise capacity. However, for those with long COVID, the reverse is the case.
This recent study has discovered why this could be true, revealing that in individuals with long COVID, surpassing their limits leads to mitochondrial damage, diminishing resilience, and triggering a relapse of their condition.
These results are crucial when formulating advice for rehabilitation or strategies for the return to work for individuals with long-term COVID.
This content has been reissued from The Conversation under a Creative Commons license.