The vagina constitutes an internal organ with an intricate ecosystem, responsive to fluctuating hormone levels throughout the menstrual cycle, pregnancy, breastfeeding, and menopause.
Following menopause and in its aftermath, there are natural alterations in the development and operation of vaginal cells, along with changes in the vagina’s microbiome (collections of bacteria residing in the vagina).
Several women may not observe these changes, as they typically don’t induce symptoms or raise concerns. However, if any symptoms arise, they are usually manageable.
Discover how your vagina changes with age, whether you’re aware of it or not.
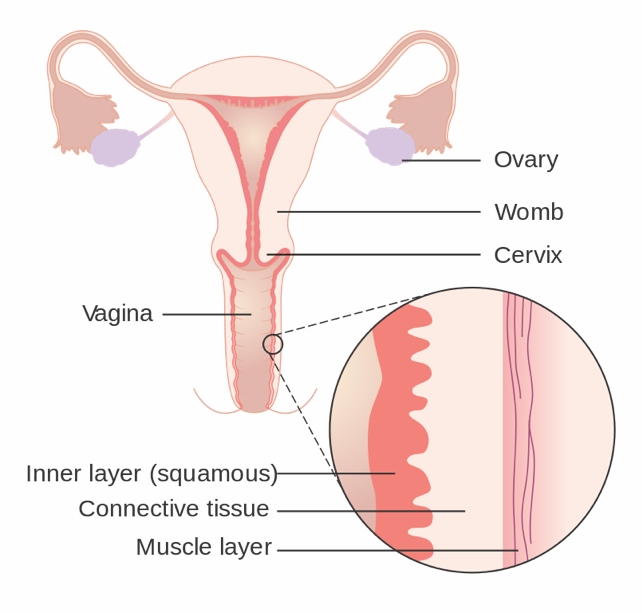
Let’s clear up the terminology
Let’s delve into the intricacies of the vagina, the muscular tube extending from the external genitalia (the vulva), through the cervix, to the womb (uterus). While the term “vagina” is occasionally used to encompass the external genitalia, it’s crucial to note that these are distinct organs with different roles in women’s health.
What happens to the vagina as you age?
Similar to numerous other organs in the body, the vagina responds to fluctuations in female sex steroid hormones during pivotal periods such as puberty, pregnancy, and menopause.
Menopause brings about a decline in circulating estrogen levels, and the hormone progesterone ceases to be produced. These hormonal shifts impact the vagina and its ecosystem. Effects may include:
- Reduced vaginal secretions, which may contribute to dryness.
- Diminished growth of surface cells in the vagina leading to a thinning of the lining.
- Changes to the support structure (connective tissue) around the vagina resulting in reduced elasticity and increased narrowing.
- Reduced blood vessels around the vagina, potentially leading to decreased blood flow after menopause. Learn more.
- A change in the type and balance of bacteria, influencing vaginal acidity, may shift from more acidic to more alkaline. Explore more.
What symptoms can I expect?
Most women may not experience noticeable or bothersome vaginal changes as they age. Additionally, there is limited evidence suggesting that these changes directly lead to vaginal symptoms. For instance, there is no conclusive evidence indicating that these changes result in vaginal infection or bleeding in menopausal women.
After menopause, some women may experience vaginal dryness, possibly due to a decrease in vaginal secretions. This can result in discomfort and pain during sexual intercourse.
However, the exact contribution of menopause to this dryness remains unclear, as younger women also frequently report similar concerns. In a study, approximately 47% of sexually active postmenopausal women and around 20% of premenopausal women reported experiencing vaginal dryness.
Changes in hormone levels after menopause also impact organs near the vagina, such as the bladder and urethra. Some women may experience recurrent urinary tract infections, leading to pain and irritation, including pain to the side of the body. It’s important to note that these symptoms are not originating from the vagina itself but are related to changes in the urinary tract.
Not everyone has the same experience
Women differ in their awareness and response to vaginal changes, and whether they are affected by them to the same degree. For instance, women experiencing vaginal dryness who are not sexually active might not observe the shift in vaginal secretions post-menopause. However, there are cases where women notice severe dryness impacting their daily functioning and activities.
Indeed, researchers worldwide are increasingly acknowledging women’s experiences during menopause to guide future studies. This involves prioritizing symptoms that hold significant importance for women, such as vaginal dryness, discomfort, irritation, and pain during sex.
If symptoms bother you
Common symptoms like dryness, irritation, or pain during sex can typically be well-managed. Lubricants can help alleviate pain during sexual activity, while vaginal moisturizers can address dryness. Both are easily accessible over the counter at your nearby pharmacy.
Despite numerous small clinical trials on individual products, these studies lack the statistical power to conclusively prove their effectiveness in alleviating vaginal symptoms.
In contrast, there is strong evidence indicating that vaginal estrogen is effective in addressing vaginal dryness and reducing pain during sex. It also lowers the risk of recurrent urinary tract infections. You can consult with your doctor for a prescription.
Vaginal estrogen is typically applied using an applicator, two to three times a week. Minimal absorption into the bloodstream makes it generally safe, but longer-term trials are needed to confirm its safety for extended use beyond a year.
Women with a history of breast cancer should consult their oncologist to discuss the suitability of using estrogen, as it may not be appropriate for them.
Are there other treatments?
Ongoing research is exploring novel treatments for vaginal dryness. One focus is on advancing our understanding of how the vaginal microbiome adjusts and evolves in response to changes in hormone levels, both circulating and local.
For instance, a limited number of reports suggest that combining vaginal probiotics with low-dose vaginal estrogen can enhance vaginal symptoms. However, further evidence is required before recommending this.
Where to from here?
The typical aging process, along with menopause, impacts the vagina as we grow older.
While the majority of women do not experience bothersome vaginal symptoms during and after menopause, for some, these may lead to discomfort or distress.
Although hormonal treatments like vaginal estrogen are an option, there is a significant demand for additional non-hormonal treatments.
This article has been reissued from The Conversation under a Creative Commons license.